What is Knee Arthritis?
Partial Knee Replacement
3D Surgical Animation
Tibial Tubercle Osteotomy – Fulkerson Procedure
3D Surgical Animation
The knee is the largest and one of the most complex joints in the human body. It consists of 4 bones, multiple ligaments, muscles and tendons, cartilage and soft tissue. The boney structures of the knee consist of the patella (knee cap), Femur (thigh bone), Tibia and Fibula (lower leg bones). The smoothness motion of the knee is accomplished through articular cartilage and fibrocartilage. Articular cartilage is the protective covering over the ends of the bones. Meniscus is the additional form of cartilage within the knee called fibrocartilage. The purpose of your two meniscuses (medial – inside and lateral – outside) is to act as cushions between your femur (thigh bone) and tibia (lower leg bone). Both kinds of cartilage allow the joint to glide permitting fluid motion during active and passive activities. The breakdown of either one of these cartilaginous structures can advance arthritic changes.

Articular Cartilage
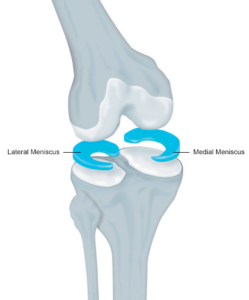
Medial and Lateral Meniscus – Fibrocartilage
There are several types of arthritis and your physician will need to determine which joint is effected and by which type of arthropathy. Osteoarthritis or “wear and tear” by definition is inflammation of a joint. When the process of cartilage breakdown begins and progresses, the joint will become stiff and painful. Osteoarthritis can occur in any active or non-active individual but usually affects individuals over the age of 50 but can be seen in earlier aged individuals depending on their occupation or their specific sport.
End-stage Osteoarthritis
Post-Traumatic Osteoarthritis
Post-traumatic osteoarthritis is an additional form of the condition that is specifically caused by a traumatic event such as a fracture or trauma such as a patella dislocation or repetitive subluxations, Ligamentous injuries, meniscus tears and surgical procedures.
Avascular
Avascular necrosis can also contribute to osteoarthritic changes within the knee. This condition is caused by the decrease in blood supply to either the distal femur (thigh bone) or the tibial plateau (shin bone). Without blood supply to a bone, the cells that maintain its strength die. This will cause collapse of the bone leading to changes within the articular surface and joint.
Osteochondritis Dissecans
Osteochondritis Dissecans or OCD lesion is a condition that can occur and develop in children, adolescents and young adults from a decreased blood supply to a specific area of bone effecting the cartilage site. The lack of blood supply causes the cartilage to become damaged and crack and loosen. This does occur in other joints of the body, but is more common in the knee. In cases of traumatic injury or in older patients these defects can be surgically repaired or replaced through procedures in which cartilage is transplanted from a cadaver or your own cartilage is grown in a lab and transplanted into the area of defect. Below is a photo of a typical OCD lesion within the knee.

Rheumatoid Arthritis
Rheumatoid Arthritis is a systemic inflammatory condition of the joint lining, or synovium. It can affect people of any age and usually affects multiple joints on both sides of the body. Once your physician evaluates you and has determined the possibility of this type of arthritis one will be referred to a specific physician that treats rheumatological diseases.
Symptoms
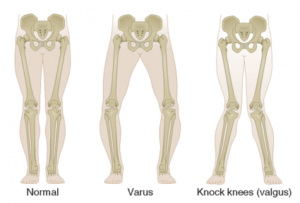
Symptoms can vary for each individual but specifically start with deep aching pain that can be aggravated by activity. This pain can radiate throughout the knee complex as well as into the proximal shin and distal thigh. Snapping, popping and even grinding will be associated with knee range of motion that will be decreased compared to a non-arthritic knee. You may also noticed that the alignment of the knee changes and becomes varus “knocked kneed” or valgus “bow legged.” Night pain is common.
Diagnosis
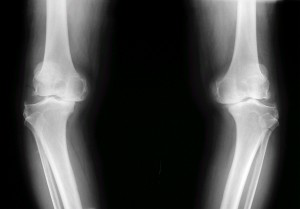
Diagnosis will be determined through a thorough history and physical examination by a trained sports medicine and orthopedic shoulder specialist. Examination will consist of palpating the knee complex for pain and a visual examination for deformities. The clinician will check both active and passive range of motion and utilize specific manual tests to determine if additional conditions exist. X-rays of the knee complex will be ordered to determine the severity of the osteoarthritic changes.
Non-Surgical Treatment or Conservative Management
Non-surgical treatment or conservative management goals are to decrease painful symptoms allowing individuals improved abilities to perform activities of daily living and labor tasks. Management consists of rest, change in activities, anti-inflammatory (NSAID) medications, Ice 20-30 minutes at times, physical therapy/home exercise program and possible injections of corticosteroid, synthetic chondroitin, stem cell or platelet plasma rich (PRP). If you have rheumatoid arthritis, your doctor may prescribe a disease-modifying drug, such as methotrexate, or recommend a series of corticosteroid injections. Dietary supplements, such as glucosamine and chondroitin sulfate (Note: The U.S. Food and Drug Administration does not test dietary supplements. These compounds may cause negative interactions with other medications. Always consult your doctor before taking dietary supplements)
Surgical management includes several options including knee arthroscopy or knee replacement.
- Knee arthroscopy, menisectomy, chondroplasty, microfracture, synovectomy, loose body removal and diagnostic evaluation, occurs when a small camera is placed into the knee joint to visualize the damage. During the diagnostic visualization, ligaments, bones and muscles of the knee complex are further assessed by the orthopedic surgeon to determine if you’re a candidate for any additional procedures such as a cartilage transplant procedure or partial knee replacement. Once the assessment has been completed the surgeon uses a variety of instruments to perform:
- partial menisectomy – removal of torn meniscal cartilage – fibrocartilage
- chondroplasty – reshaping of articular cartilage
- joint debridement -removal of loose fragments
- synovectomy – debridement or removal of inflamed synovial tissue (joint lining)
- microfracture – in specific cases of OCD lesions this may be performed. This is a process in which the defect of bone where articular cartilage has broken away is picked to release bone marrow stem cells to build a fibrinous cartilage cap to improve pain and mobility.
This is an outpatient procedure.
- Osteotomy is a procedure performed to change the alignment of the knee to take pressure off an area or arthritic decline. This can either be done to the femur (thing bone) or tibia (shin bone). The procedure requires the physician to cut the bone and then reshape the alignment of the knee. This procedure is also performed when implanting regrown cartilage to the trochlea or patella to avoid the same pressures that caused the initial disease process.
Tibial Osteotomy
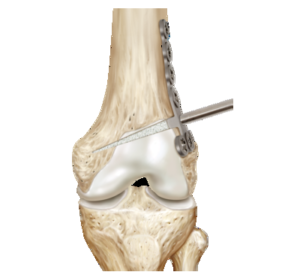
Femoral Osteotomy
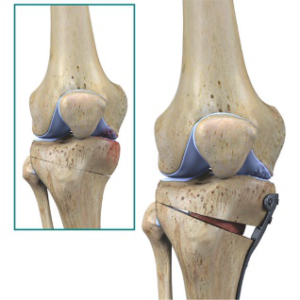
- Partial knee replacements can occur if only one of the three compartments (patellofemoral, medial and lateral) of the knee have been affected by arthritic change. In this case only one of the three compartments would be replaced.

A partial knee and total knee replacement
- Total knee arthroplasty or replacement is when all compartments are replaced with a mechanical devise. For individuals who have failed conservative treatments including arthroscopies, corticosteroid injections, supplement injections, physical therapy, bracing and activity changes this is the definitive procedure to resolve symptoms. Many joint replacements are now being performed at outpatient surgery centers. Recovery is 4-6 months.
